When Words Don’t Come: How Brain Data Supports Non-Verbal Communication in Dementia

NEMA AI
In settings across care homes, hospitals, and home-based support, a powerful challenge persists. When dementia silences verbal communication, those closest to the person must interpret subtle expressions, routine behaviors, or slight gestures to understand needs. One raised eyebrow when asked to eat might signal discomfort. A frown and tense shoulders might mean confusion. These cues are real. They are also fragile, inconsistent, and universally taxing for caregivers who must respond without certainty.
For clinical and operational leaders, the inability to accurately interpret non-verbal expressions means delays in care, unnecessary escalation, increased staffing burdens, and emotional burnout. It also threatens care quality, regulatory compliance, and institutional reputation.
Nemaai offers a compelling solution. By harnessing electroencephalography (EEG) to measure brain activity reflecting emotional and stress states, Nemaai provides objective, real-time insight into the internal world of persons with dementia. This enables caregivers to respond proactively, reducing conflict, improving comfort, and preserving human dignity.
1: The Growing Challenge of Silent Communication
Globally, over 55 million people live with dementia, and that number is expected to rise dramatically in coming decades (Alzheimer’s Association, 2024). As dementia advances, the loss of language becomes inevitable. The reasoning center may still work. A spark of recognition may still dwell behind the eyes. But the ability to communicate it often fades.
For a family caregiver this might mean watching a spouse search for a word. For facility staff, it could mean charting repetitive questions or behavioral outbursts with no apparent trigger. Without reliable communication pathways, caregivers are making high-stakes decisions with low data. That is not sustainable. Nor is it safe.
In behavioral terms, agitation might lead to over-medication. Resistance in personal care might be interpreted as deliberate instead of fear. Quiet moments might be taken for peace when they are actually signs of discomfort. These misreadings escalate caregiver burden and risk.
Organizations need a better way to understand without relying on speech. They need data that respects the person but empowers care. That is the promise of EEG emotion tracking.
2: Why Non-Verbal Cues Often Fall Short
Non-verbal communication includes facial expression, body posture, breathing, changes in tone, and the context of behavior. Family members often develop intuition for their loved one’s cues. A hand lifted in a particular way may mean craving. A look out the window may mean longing. After years of observation, many family caregivers learn to translate these cues effectively.
In professional care environments, that depth of familiarity rarely exists. Staff are trained to notice broader signals, but not idiosyncratic patterns. In busy care homes or hospital units, staff rotate, shifts change, and real continuity of insight is rare. Add to that cultural differences, stoicism, and personality, and the same behavior can have different interpretations. A raised voice can be distress or invitation. Pacing can be agitation or habit.
Inconsistent interpretation leads to inconsistent care. One caregiver may intervene with empathy, another with restraint. Over time, this fragmentation undermines trust, increases distress, and amplifies risk.
What is needed is a consistent, objective lens, one that reads internal states when behavior does not deliver the message.
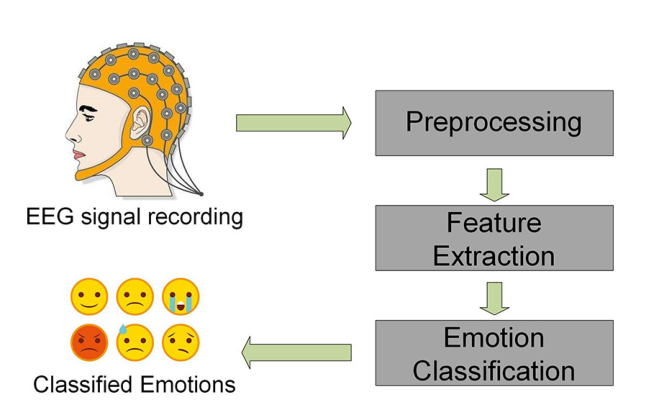
3: How EEG Captures the Emotional Brain
Electroencephalography records electrical activity across the scalp. That activity organized into brainwaves reflects cognitive and emotional processes:
- Alpha waves (8–13 Hz) often correspond to restful attention and emotional calm.
- Beta waves (13–30 Hz) reflect active mental load, focus, and sometimes stress.
- Theta waves (4–7 Hz) emerge during meditation, memory processing, or cognitive overload.
- Event-related potentials, such as the P300 measured after stimuli, show processing speed and attention capacity.
For people unable to express their internal state verbally, these signals are windows. Elevated beta and suppressed alpha may indicate anxiety. Theta surges can signal confusion or overload. ERP delays suggest a slowing of cognitive processing. EEG thus offers direct insight into what the person might be feeling or struggling to articulate.
4: Scientific Foundations of Emotion Tracking via EEG
Several studies validate the link between emotional or cognitive states and EEG patterns:
- In older adults, emotion recognition in reminiscence therapy correlated with EEG patterns. Researchers achieved 95 percent accuracy in distinguishing emotional responses using EEG and AI modeling (Jiang et al., 2022)
- Among Alzheimer's patients, emotion classification using EEG and machine learning identified states such as happy, peaceful, or bored with approximately 71 percent accuracy (Sensors, 2020).
- In dementia, EEG theta and alpha responses varied depending on recognition of negative emotional expressions, showing altered emotional processing (Güntekin et al., 2019).
- Emotion classification studies using CNN-LSTM approaches demonstrate that EEG can reliably differentiate emotional states, supporting real-time tracking (Hosseini et al., 2023).
- A systematic review confirmed that machine learning enables EEG to detect cognitive and emotional states across diverse populations (Saeidi et al., 2021).
These findings give confidence that brainwave data can be translated into emotional insight, not just neurophysiological noise.
5: Redesigning Care Scenarios with EEG Insight
Avoiding Morning Agitation in a Memory Care Unit
A resident consistently wakes feeling unsettled. Without words, the behavior looks like agitation and the response becomes sedation. With EEG monitoring, care staff see beta increases before the resident starts calling out. A soft light and gentle reassurance interrupts the escalation. The resident calms, easing morning routines.
Understanding Resistance in Personal Care
A hospital patient pulls back when asked to move. By pattern, staff perceive confusion or resistance. EEG shows elevated theta and slow ERP signals, suggesting cognitive overload. The caregiver changes to simpler sentences and calming tones. The patient cooperates. Sedating medications are avoided.
Supporting Home-Based Dignity
An elderly person living alone with dementia often becomes restless in the evening. A wearable EEG flags stress markers 30 minutes before pacing begins. A mobile alert prompts the caregiver to offer a snack and reduce lighting. The person stays calm through the night.
These use cases reveal more than reduced incidents. They show enhanced understanding, faster response, and preservation of autonomy.

6: Business Value for Care Providers and Tech Integrators
For operational leaders and healthcare executives, EEG-enabled care offers measurable advantages:
- Reduction in emergencies and falls: Early intervention reduces crisis events.
- Lower medication use: Instead of sedation, care becomes personalized intervention.
- Improved staff retention: Confidence rises when caregivers feel guided, reducing burnout.
- Better documentation: Emotional state metrics strengthen quality logs and audits.
- Competitive differentiation: Facilities can promote brain-informed care as innovation and empathy.
These outcomes suggest risk reduction and better quality indexing. Tech integrators can embed emotion-tracking features into EHR systems or nurse call tools as enhanced service offerings.
7: Deployment Strategy for Institutions
Implementing EEG-based emotion tracking requires careful alignment across technology, people, and policy:
Device Design and Fit
Wearable EEG headbands must be lightweight, comfortable, stable during movement, and easy to sanitize. Stakeholders must ensure sensor reliability and minimal care disruption.
Data Processing
Real-time AI models process raw EEG into emotion flags agitated, calm, confused.
Consent and Privacy
Residents or their legal representatives need to consent ahead of monitoring. Consent should be reaffirmed regularly. EEG data is encrypted, anonymized, and retained under health data protections.
Model Validation and Adaptation
AI models must be validated for diverse populations. Institutions should provide feedback loops if alerts are incorrect, caregivers can flag and help retrain the model.
This structured approach ensures technical integration, ethical use, caregiver readiness, and organizational alignment.
8: Ethical Considerations
When reading brain states, the ethical stakes are real.
Consent integrity is vital with cognitively impaired individuals. Consent workflows must be robust and inclusive.
Privacy protections must exceed those of behavioral sensors. Emotion tracking must not identify personality traits or mental health beyond real-time state.
Avoiding overdependence is crucial. Caregivers must not rely solely on data. Alerts should complement observation, not replace human empathy.
Transparency in algorithm behavior helps build trust. Caregivers and families should understand what the data means and its limitations.
Nemaai builds with these principles at the core, partnering with ethicists and clinicians during design and rollout.

9: Nemaai’s Unique Strengths
- Edge processing: The device processes data locally, sending only state summaries strengthening data security and reducing infrastructure needs.
- Intuitive caregiver interface: Alerts are clear and actionable, without labeling emotions in reductive terms.
- Ethics and consent embedded: Consent, data governance, and feedback mechanisms are designed into workflows, not bolted on.
These factors combine to deliver technology that enhances empathy, not replaces it.
10: A Silent Revolution in Dementia Care
In the future, we may see:
- Wearable brain-state monitors integrated with smart environments.
- Predictive analytics foreseeing agitation hours in advance.
- Remote caregiver support with emotional data guidance.
- Tailored interventions music, light, movement triggered by brain signatures.
What remains constant is humanity. The goal of Nemaai is not to create emotion, but to perceive it when words no longer surface. To support caregivers in truth-seeking. To ensure dignity when speech fades. This is the silent revolution in dementia care, a shift from interpreting behavior to understanding the brain, from managing symptoms to honoring presence.
At NEMA AI, we’re building technology that gives a voice to those silent mental states.
Using safe, non-invasive EEG headsets, we capture the brain’s real-time activity to detect
Want to learn more?
Book a demo or in-person session today in Delhi, Hyderabad, Mumbai, or Bangalore.
Suggested by NEMA AI
A PSYCHOMETRIC TEST THAT CAN NOT BE FAKED
Psychometric tests have long been utilized to gain insight into an individual’s cognitive abilities, personality traits,
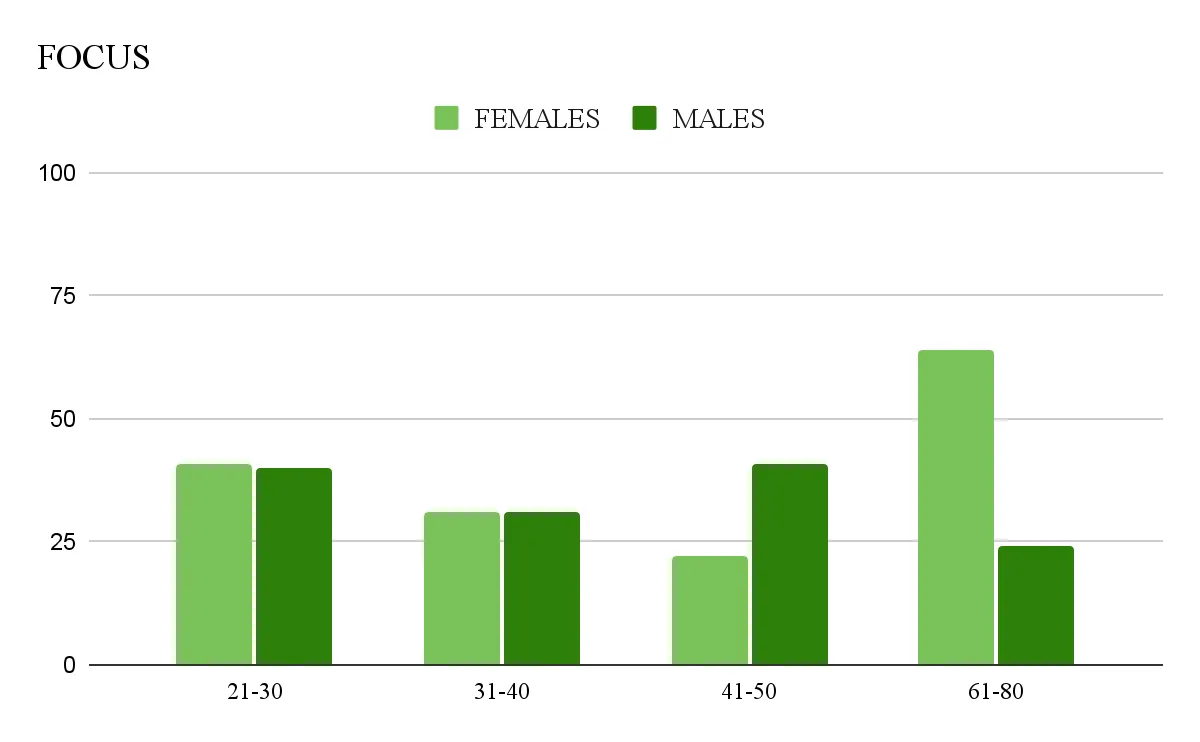
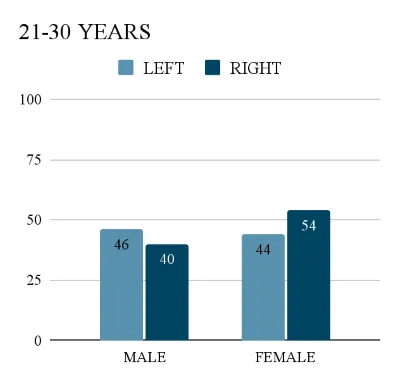
Exploring Age and Gender Differences in the Fields of Attention and Focus
The capacity to keep your attention and focus is an essential talent in a fast-paced, distracted society. However, level