What Does Confusion Feel Like? Tech That Listens to the Brain

NEMA AI
Dementia is the progressive loss of cognitive functioning like thinking, remembering, it interferes with a person’s day to day activities.
Many a times, controlling their emotions is not up to the person and there are different ranges of severity for dementia like the mildest stage which is the beginning stage to the most severe where a person has to depend on someone else for walking and feeding them (National Institute on Aging).
Many people confuse dementia with Alzheimer's disease. Dementia can be caused due to a lot of diseases, one of the most common being Alzheimer's disease.
Dementia is said to be caused mostly as a result of the alterations in the brain that causes nerve cells and the connections to not perform ideally (Kumar et al., 2024).
Cognitive confusion in dementia
From a clinical and patient perspective a person might have apathy, emotional withdrawal, having trouble with solving familiar tasks, memory loss that erupts in their daily life.
Even though the human lifespan has increased drastically in the last few decades, the rates of cognitive pathology have increased drastically too. It has been estimated that around 75 million people by 2030 will have dementia (Dinius et al., 2023).
Brain fog is not to be confused with dementia which happens in a lot of cases. Brain fog is typically a temporary state where a person has diminished mental clarity and thought while dementia is a decline in the cognitive state(Ocon, 2013).
A lot of the time, caregivers dismiss dementia as a natural part of aging, or they neglect it by saying that it is a personality trait like being moody or stubborn.
Limitations regarding Dementia care
Traditional cognitive screening tools like the Mini-Mental State Examination (MMSE) are widely used, but they come with significant limitations especially in detecting early or atypical forms of dementia. These tests rely heavily on verbal responses, reading, writing, and short-term memory tasks, which can miss cognitive changes related to executive dysfunction, emotional regulation, or visuospatial ability (Panegyres et al., 2016).
Moreover, MMSE scores are often influenced by a person’s age, education level, and language proficiency, leading to both false positives and false negatives (Piersma et al., 2018). In highly educated individuals, early symptoms may go unnoticed (a ceiling effect), while in low-literacy populations, normal aging may be misread as pathology (Li et al., 2018).
For non-verbal patients or those with physical impairments, these tools become inaccessible altogether (Carnero-Pardo, 2014), As a result, early and meaningful signs of confusion or cognitive fatigue are often overlooked highlighting the need for more inclusive, objective tools like EEG-based brain monitoring.
EEG and why does it matter?
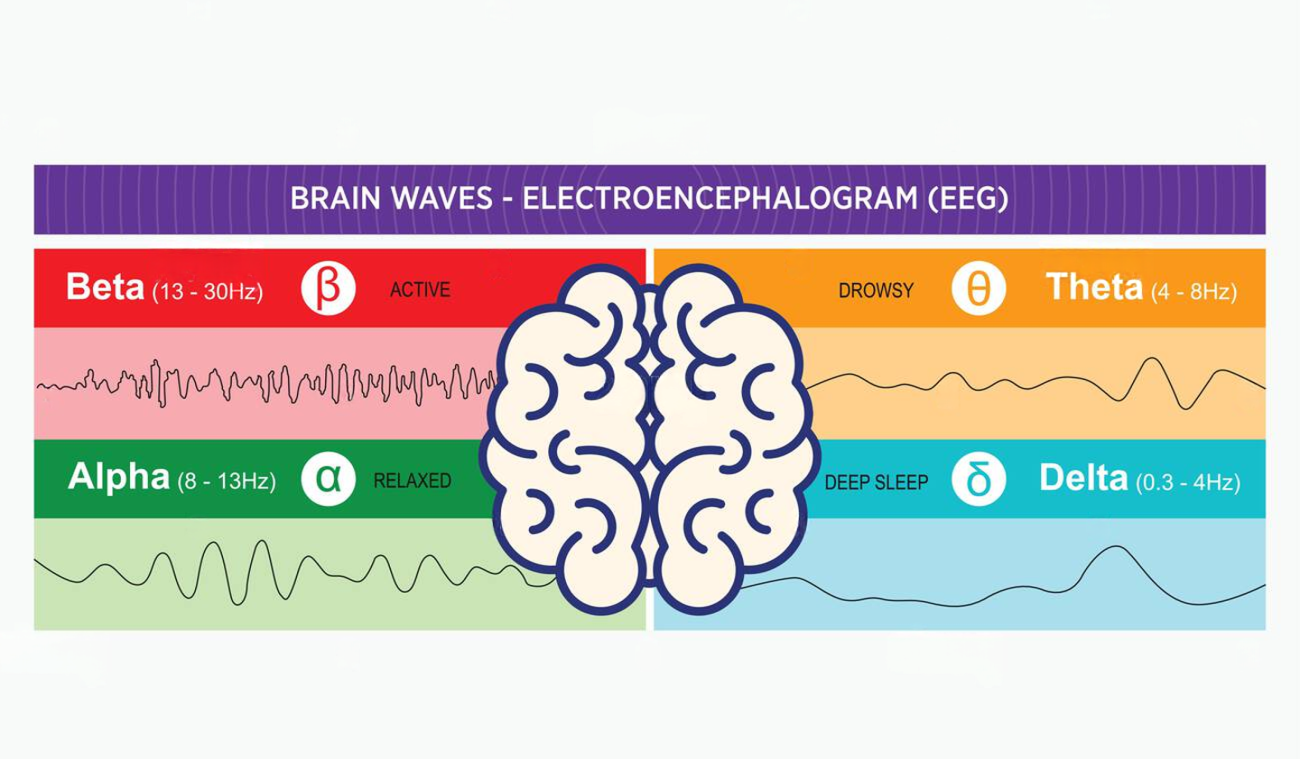
Electroencephalography, or EEG, is a safe, non-invasive method that records electrical activity in the brain using sensors placed on the scalp. These signals called brain waves are used to monitor how the brain is functioning in real time (Blocka & Yetman, 2012).
Different types of brain waves correspond to different mental states: for instance, beta waves (13–30 Hz) are linked to active thinking and alertness, alpha waves (8–12 Hz) appear during relaxed but wakeful states, and theta waves (4–8 Hz) emerge during drowsiness or early sleep. When someone is experiencing cognitive overload, mental fatigue, or confusion, EEG may reveal a shift from high-frequency beta activity to slower alpha or theta waves indicating reduced attention and processing capacity (Attar, 2022).
These changes are especially relevant in early dementia, where patients may struggle to express how they feel. By detecting these subtle shifts in neural activity, EEG offers a unique window into mental states that are often invisible to conventional screening tools.
How does it help?
Many individuals affected by neurological or psychiatric conditions struggle to communicate their internal experiences whether due to advanced dementia, autism spectrum disorders, or trauma-related non-responsiveness. In such cases, traditional cognitive assessments, which rely on speech, writing, or task performance, often fail.
EEG-based brain monitoring, like the solutions developed by NEMA AI, offers a breakthrough. By recording real-time electrical activity from the brain, EEG can detect mental states like cognitive fatigue, emotional withdrawal, and confusion even when the patient is non-verbal or behaviorally unresponsive (Trapp et al., 2022).

In autism, for example, altered EEG signatures have been linked to differences in sensory processing and attention (Marta Elena Santarone et al., 2023). Similarly, in dementia, EEG can pick up changes in brain connectivity before symptoms are visible in behavior or speech. Non-verbal brain monitoring is not only more inclusive, but also more objective and scalable, empowering caregivers and clinicians with insights they would otherwise miss ensuring patients are heard, even when they cannot speak (Yen et al., 2023).
AI integration
Raw EEG signals are complex, high-dimensional, and often noisy making interpretation a challenge for clinicians. This is where Artificial Intelligence (AI) plays a transformative role. By applying advanced machine learning algorithms, AI can identify patterns in brainwave data that may not be visible through traditional analysis (Saeidi et al., 2021).
These models can learn to distinguish between normal and abnormal cognitive states such as mental fatigue, early confusion, or emotional withdrawal with high accuracy and in real time. In the context of dementia, AI-driven EEG analysis can detect early biomarkers of neurodegeneration before clinical symptoms emerge, enabling earlier interventions (Hussein Ali Hamzah & Abdalla, 2024).
At NEMA AI, we integrate AI with EEG to automate and personalize brain assessments, removing subjectivity and making cognitive health insights accessible even in non-clinical settings. Ultimately, AI bridges the gap between brain data and actionable understanding making non-verbal brain signals speak volumes.
Early detection and the tools that will help
Early detection of dementia can profoundly alter the course of care enabling timely medical intervention, access to cognitive therapies, and crucially, allowing families to prepare and adapt to evolving needs. According to the (World Health Organization, 2019), early diagnosis leads to better outcomes, reduces healthcare costs, and improves quality of life for both patients and caregivers.
However, traditional tools often fail to detect subtle cognitive decline in its earliest stages especially when patients can’t articulate their struggles (Chun et al., 2021).
This is where NEMA AI steps in. Using non-invasive EEG technology, NEMA AI detects shifts in brainwave patterns linked to confusion, fatigue, and attention deficits, offering objective, real-time insight even in non-verbal or cognitively impaired individuals. It's not just tech, it's a way to understand what words can no longer express, giving families and clinicians a chance to act when it still matters most.
At NEMA AI, we’re building technology that gives a voice to those silent mental states.
Using safe, non-invasive EEG headsets, we capture the brain’s real-time activity to detect
Want to learn more?
Book a demo or in-person session today in Delhi, Hyderabad, Mumbai, or Bangalore.
Suggested by NEMA AI
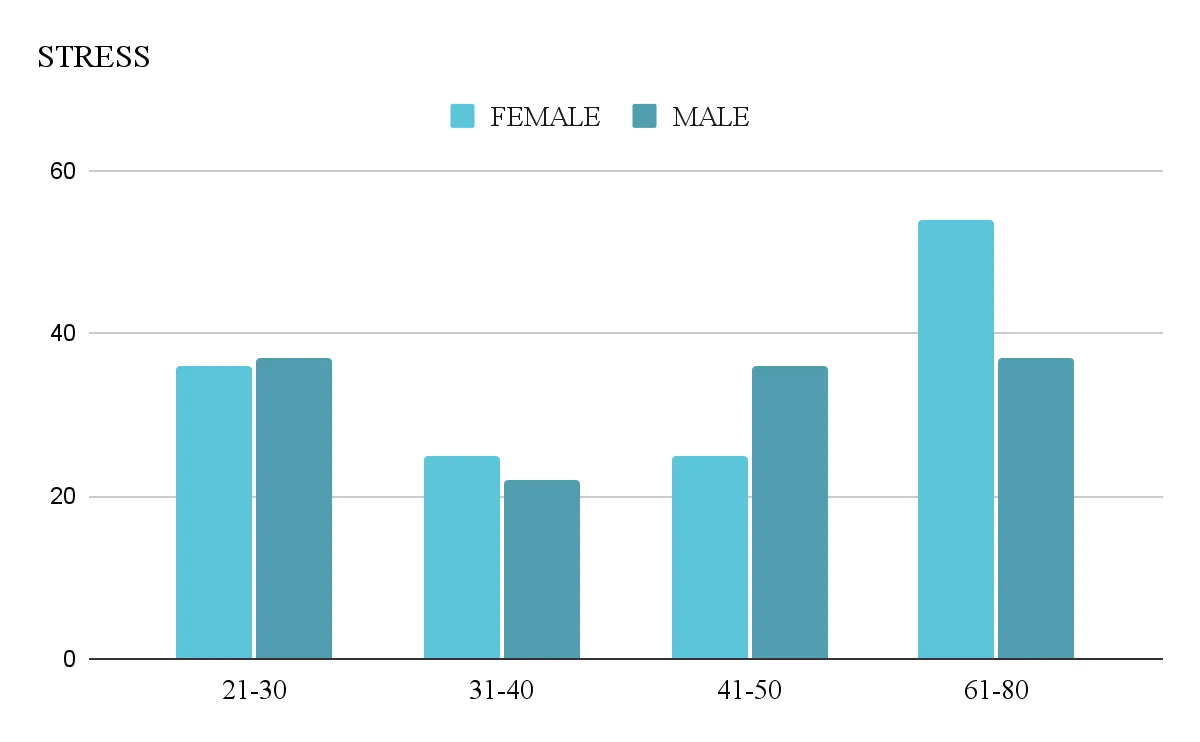
Exploring Stress, Thinking & Interaction Levels using NEMA AI.
NEMA AI, a New Delhi, India-based startup merging neuroscience and AI to revolutionize mental health care.Our research o

Unleash Your Potential: NEMA AI’s In-Person Career Guidance and Counseling Session
Embarking on a journey of self-discovery is a transformative experience, especially when it comes to your career. NEMA A